-
Posts
594 -
Joined
-
Last visited
Content Type
Profiles
Blogs
Forums
American Weather
Media Demo
Store
Gallery
Posts posted by sokolow
-
-
Preprint of “Coronavirus Disease Outbreak in Call Center, South Korea“ by Park and co.
https://wwwnc.cdc.gov/eid/article/26/8/20-1274_article
Via Zeynep Tufekci (@zeynep) From perspective of what does it imply for normal people, she points out for us both disturbing and reassuring potential findings claimed in paper: on one side of the floor, damn near half of the staff were infected; much lower transmission at home, low transmission to other floors. Very few infected persons (~2%) failed to show clinical signs within 14 days.
She points out that like we talked about upthread, highest risk situation is crowding, or rather, prolonged mutual exposure while indoors.
-
 1
1
-
 1
1
-
-
I wonder if this will verify
Trevor Bedford says
-
-
A friend sent along this NYT letter which talks about happy hypoxics, and boy this excerpt really is “a day in the life”
https://www.nytimes.com/2020/04/20/opinion/coronavirus-testing-pneumonia.html
QuoteDuring my recent time at Bellevue, though, almost all the E.R. patients had Covid pneumonia. Within the first hour of my first shift I inserted breathing tubes into two patients.
Even patients without respiratory complaints had Covid pneumonia. The patient stabbed in the shoulder, whom we X-rayed because we worried he had a collapsed lung, actually had Covid pneumonia.
-
9 hours ago, Hoosier said:
Has anyone been able to find hand sanitizer? I seriously think I'd have a much better shot at striking oil in my backyard right now.
i’ve been cutting isopropanol with aloe vera gel 3:1
-
 1
1
-
 1
1
-
-
Here’s the study from China that was floating around
“Our study does not rule out outdoor transmission of the virus. However, among our 7,324 identified cases in China with sufficient descriptions, only one outdoor outbreak involving two cases occurred in a village in Shangqiu, Henan. A 27-year-old man had a conversation outdoors with an individual who had returned from Wuhan on 25 January and had the onset of symptoms on 1 February.”
I didn’t see that they characterized the details of the conversation in terms of proximity, weather, shared touch of each other or objects/surfaces
https://www.medrxiv.org/content/10.1101/2020.04.04.20053058v1.full.pdf
medxriv preprint, Indoor transmission of SARS-CoV-2 by Qian, et. al
They give details of four representative indoor events: supermarket, family affair, mall, and i forget, but the family gathering caught my eye: 19 present, 11 infections [!]
“Nineteen members of three families, including two relatives from Guangdong, who attended a hotpot family gathering at Lento Party Room on 26 January. Eleven were infected; the first case showed symptoms on 30 January. The venue has a hotpot area, BBQ space, mahjong table, ping pong table, pool table, and karaoke.“
Which is striking because as IL found out with the family gathering transmission event that got analyzed, going around and saying hi to everyone is a great way to blow up a bunch of infections
...
And the popsci article roundups were flogging this, which has a great line in the intro and cool imaging of our gross human aerosol sprays
“The use of a tissue (in this case, 4-ply, opened and ready in the hand) proved to be surprisingly effective, though the effectiveness of this depends on the tissue remaining intact and not ripping apart”
which IMO is a lovely line because of how viscerally you can imagine the sensation of letting loose a nasty blast, both barrels mouth and nose, and blowing a BRAWNY BRAND paper towel right the f apart and then you got a handful of sneeze, snot, and shredded paper towel in your hand
https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0021392
Qualitative Real-Time Schlieren and Shadowgraph Imaging of Human Exhaled Airflows: An Aid to Aerosol Infection Control by Tang and company
bonus pic “For some experiments, two subjects may face each other across the mirror in order to visualize how their exhaled airflows interact during, e.g. during normal conversation”

i think the takeaway whichever mag WIRED? OutsideOnline? had on the outdoors activity thing and the slipstream thing was “probably the risk of biking or running near someone is overstated but don’t hang out upwind or downwind of people”
edit yup it was WIRED
https://www.wired.com/story/are-running-or-cycling-actually-risks-for-spreading-covid-19/
-
 1
1
-
-
I don’t think there’s really any hard answers that I’ve heard, and I gather that the question is still an active topic of investigation for the flu. Podcast I was listening to points out its winter-summer seasonal in temperate latitudes, and appears to tend towards rainy / dry seasonal in tropical latitudes, although both types of climate regions experience flu epidemics, and at least in the places where they’d looked, the tropics may experience the same rates of infection. It may be related to there being a sweet spot for transmission as far as temp & humidity goes; they were also saying of course it may simply have a lot to do with how much time people tend to spend indoors and in close proximity to one another
With the ‘rona I think the word is no-one really knows how different transmission dynamics are to the flu. The major spreading events that have been documented & studied were looked at by researchers in China, and they found that virtually all of the transmission cases they tracked were indoors but there were a bunch of caveats, namely its a shared environment right? And before indoor/outdoor come definitively into play you have to consider proximity, density of people, and time. IIRC it was pointed out that the study was done in a polity with strict stay-at-home and social distancing measures, so it doesnt rule out that the big factor might be, basically, crowding
-
-
8 hours ago, sokolow said:
Really looking forward to a sunny, breezy day
TRIP REPORT its fantastic here on the South Side
-
Bedford thinks aloud in this thread about the potential differences between the Seattle and Santa Clara results
He points out he has operating with the educated working assumption that untraced infections are something like 10-20x confirmed cases, but is eager for more data to give foundation to or revise that number range
QuoteEstimating total number of infections is difficult without serology (see this thread: https://twitter.com/trvrb/status/1247609734896607232…), but I'd guess that we're catching between 1 in 10 to 1 in 20 infections as a confirmed case. 14/18
He also highlights this discussion by biostats prof Natalie Dean on her critical first read of the Santa Clara study
-
Trevor Bedford, PI at the eponymous Bedford lab at Fred Hutch out Washington way highlights the first look at results from the Seattle area ‘rona prevlance study.
The technical report is a good read because it walks the reader through the caveats and possible confounding factors of their methodology and the resulting data
PDF link
https://publichealthinsider.com/wp-content/uploads/2020/04/SCAN-Technical-Report-v1-17-APR-2020.pdf
Both of those links from this thread, which is worth a read
QuoteOn March 23, Public Health — Seattle & King County and the team behind the Seattle Flu Study launched the greater Seattle Coronavirus Assessment Network—or SCAN for short. Thanks to the participation of volunteers across the county, SCAN has already begun to identify cases that might otherwise have gone undetected.
In its first 18 days, SCAN tested 4,092 samples. Nearly two-thirds of those were returned by individuals who in the seven days prior to enrollment had reported COVID-like illness (fever, cough, or shortness of breath). However, more than three-quarters of these individuals indicated they had not yet sought medical care. SCAN is the first COVID-19 surveillance program in the U.S. to use “swab-and-send” test kits that allow individuals to collect their own nasal sample and return it to a lab for testing without leaving home—while observing physical distancing guidance and reducing exposure to others.
SCAN testing among those reporting COVID-like illness (CLI) returned 44 (1.6%) positive results for COVID-19—a proportion lower than that being returned through testing within the medical system, but one that may still represent thousands of unrecognized infections in the community.
-
 1
1
-
-
-
Really looking forward to a sunny, breezy day
-
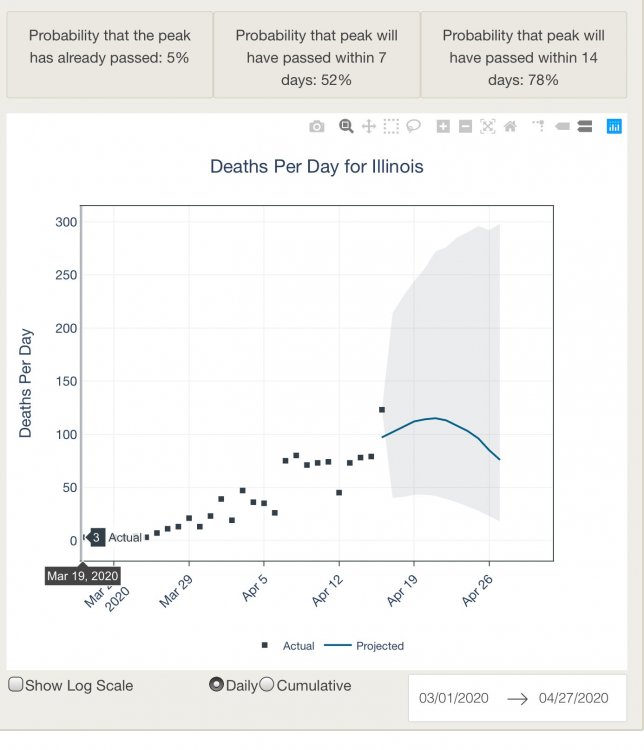
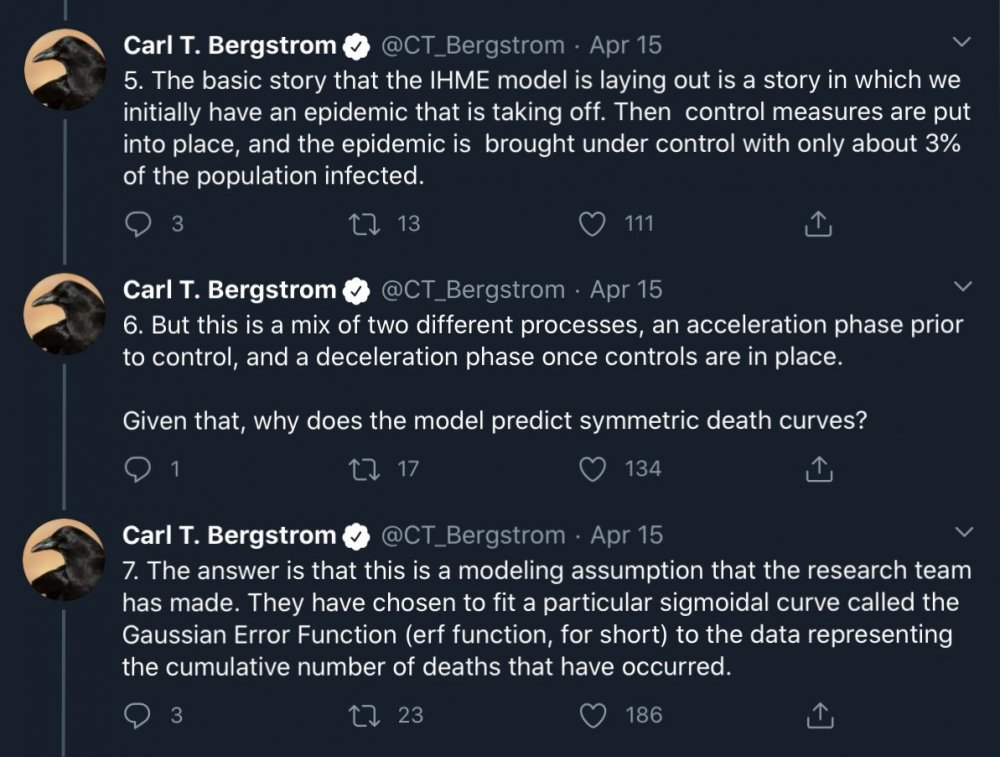
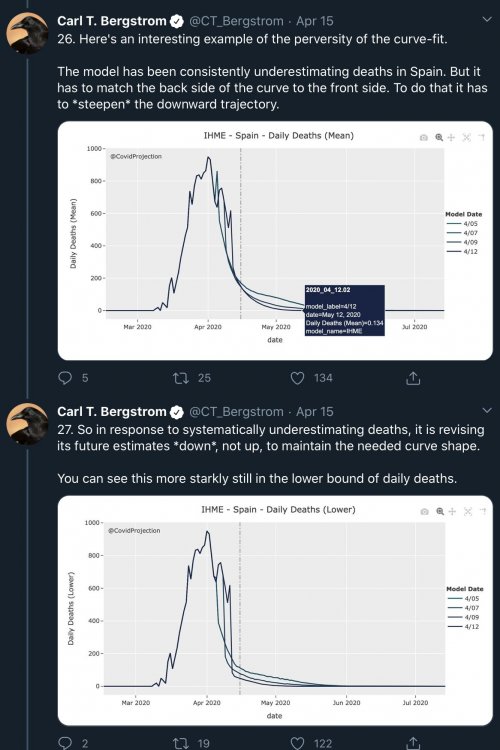
if anyone else is following that whole deal with the IHME model there’s this
and the viewer is here
https://covid-19.tacc.utexas.edu/projections/
On March 26, 2020, the Institute for Health Metrics and Evaluation (IHME) at the University of Washington released a website that forecasts coronavirus disease (COVID-19) healthcare demand and mortality for all states in the United States. After being cited during a White House briefing on COVID-19 modeling efforts, their forecasting model, described in a preprint on medRxiv [IHME et al., 2020], has received an enormous amount of attention from both the general popula- tion and scientific community. IHME has since updated the model several times resulting in considerable revisions to the COVID-19 forecasts.
The IHME approach departs from classic epidemiological modeling. Rather than using systems of equations to project the person-to-person transmission of the virus, the model postulates that COVID-19 deaths will rise exponentially and then decline in a pattern that roughly resembles a bell curve (i.e., normal distri- bution). The model assumes that the shape of the curve will be curtailed by so- cial distancing measures. Key inputs driving this component of the IHME model include the reported dates of state-wide shelter-in-place orders and shapes of COVID-19 epidemiological curves observed in Chinese and European cities fol- lowing the implementation of similar measures.In light of the popular appeal of the IHME model and considerable scrutiny from the scientific community, we have developed an alternative curve-fitting method for forecasting COVID-19 mortality throughout the US. Our model is similar in spirit to the IHME model, but different in two important details.
1. For each US state, we use local data from mobile-phone GPS traces made available by SafeGraph to quantify the changing impact of social-distancing measures on “flattening the curve.” SafeGraph is a data company that ag- gregates anonymized location data from numerous applications in order to provide insights about physical places. To enhance privacy, SafeGraph excludes census block group information if fewer than five devices visited an establishment in a month from a given census block group.
2. We reformulated the approach in a generalized linear model framework to correct a statistical flaw that leads to the underestimation of uncertainty in the IHME forecasts.
The incorporation of real-time geolocation data and several key modifications yields projections that differ noticeably from the IHME model, especially re- garding uncertainty when projecting COVID-19 deaths several weeks into the future. -
On 4/15/2020 at 8:56 AM, sokolow said:
In re the IHME model, here is an interesting discussion of side effects that arise from it having been designed as a resource-use forecasting tool for healthcare institutions & response planning, but then being employed “off label” as it were in a broader context
here you go, go nuts
read the whole thread tho, the whole bit is important if you’re like me & trying to follow along from the back row while people who have expert field knowledge discuss their work for laypeople & their peers simultaneously
-
 1
1
-
-
12 minutes ago, Snownado said:
I keep hearing that there could be 60,000 deaths by early August yet it seems like at least 2,000 per day are dying now. If we keep up this rate it will be over 60,000 this month. So apparently they are expecting a sharp decline in deaths very soon ?
thats what IHME forecast. upthread there’s some discussion about what specific purpose that model was designed for, what the big caveat is that is built into its premises, and why the purpose for which it was designed results in exactly the thing you described and why that’s not necessarily ideal when using the tool for other applications
-
21 minutes ago, sokolow said:
i went and had a glance and surveys have been done in denmark (evidence for prior infection found in 3% of blood donors, 4% in healthcare workers), similar numbers in netherlands, ongoing in wuhan, and also in santa clara county
glancing more as to what all that actually means for the policy questions we want to make it serve, the upshot appears to be “we don’t know yet” because there’s apparently a dozen ways these findings could be confounded or overinterpreted, and of course there is a strong appeal towards drawing the implication of a lower IFR. i am sure we’re going to hear the TWiV nerds talk about this and i can’t wait to hear an epidemiologist do an expert roundup
-
i went and had a glance and surveys have been done in denmark (evidence for prior infection found in 3% of blood donors, 4% in healthcare workers), similar numbers in netherlands, ongoing in wuhan, and also in santa clara county
-
half a percent give or take sure seems pretty low if we’re talking scratchoffs or winning the big TV at the xmas raffle but thats sh!t-high odds when the prize is death and the runner up prizes include the possibility of long-term perhaps (who knows!) permanent lung damage or a nice long stay on vent. not to mention this isnt like a slot machine we get to play alone, we’re all at the table
-
 2
2
-
-
that would be fantastic if it was true. instead its just a possibility thats plausibly true but that we really really wish was real
we know there’s a lot more infections than cases, sure. but how many more, thats the big cash prize
whats the values out of the one prevalence study that got done in heinsberg? ~15% of the persons sampled in city had been infected to date and that worked out to ~0.5% infection fatality?
-
I was posting about this guy earlier and this deep dive into the past (2 March!), as it were, is a cool read if you haven’t seen it before.
https://bedford.io/blog/ncov-cryptic-transmission/
But r/n I thought y’all might like this thread on the test - trace challenge
-
@HelenBranswell points to article by her colleagues at STAT on the U of C hinting at useful results found in early remdesivir clinical trials EDIT a friend tells me they got questions about the value of this trial because lack of control arm combined with not real clear on criteria they used for who was admitted to study.
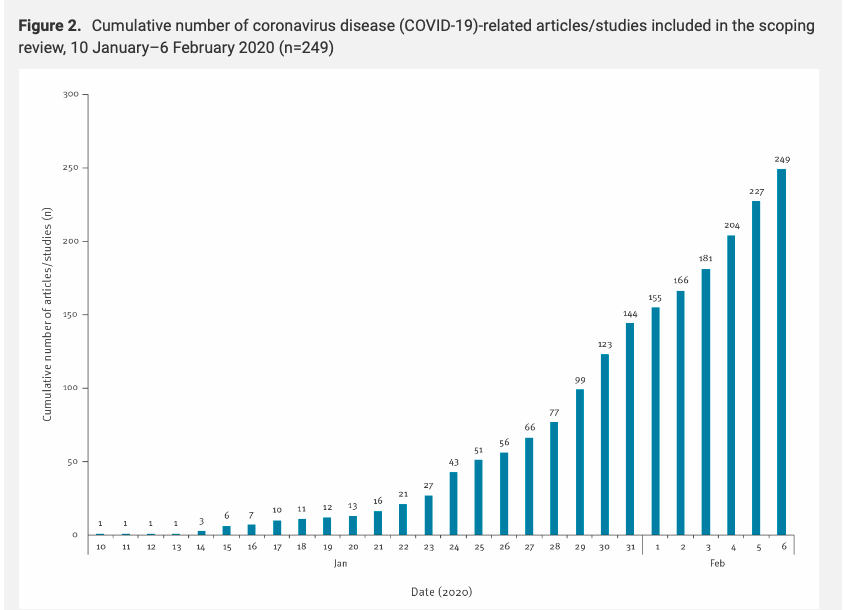
but more importantly she has discovered intriguing relationship between cumulative confirmed C19 cases, and scientific articles related to the of the covid epidemic. coincidence....? i think not ......
-
39 minutes ago, KokomoWX said:
Those who support the stay at home order, how far are you willing to keep it going? June 30th? Labor Day? January 2021? I'm just asking.
That’s kind of a nonproductive question by itself. Who wants to keep it going for fun? I think we’ve talked about this itt that the critical elements public health specialists are emphasizing that we need to have in place and functioning if we don’t want to go back to the same miserable story are Rapid test, Trace, Isolate, Treatment (overflow capacity and effective interventions) in the context of few enough active infections for the inbuilt time lag of the first two steps to not make the third useless.
I suggest the alternate question “At what point to we conclude our business, political and healthcare leadership is incompetent for failing in allowing us to build & implement this public health monitoring infrastructure” because that’s the point where we “break stay at home” to “don proper PPE“ and “dump them in Lake Michigan”
-
 1
1
-
-



Coronavirus
in Lakes/Ohio Valley
Posted
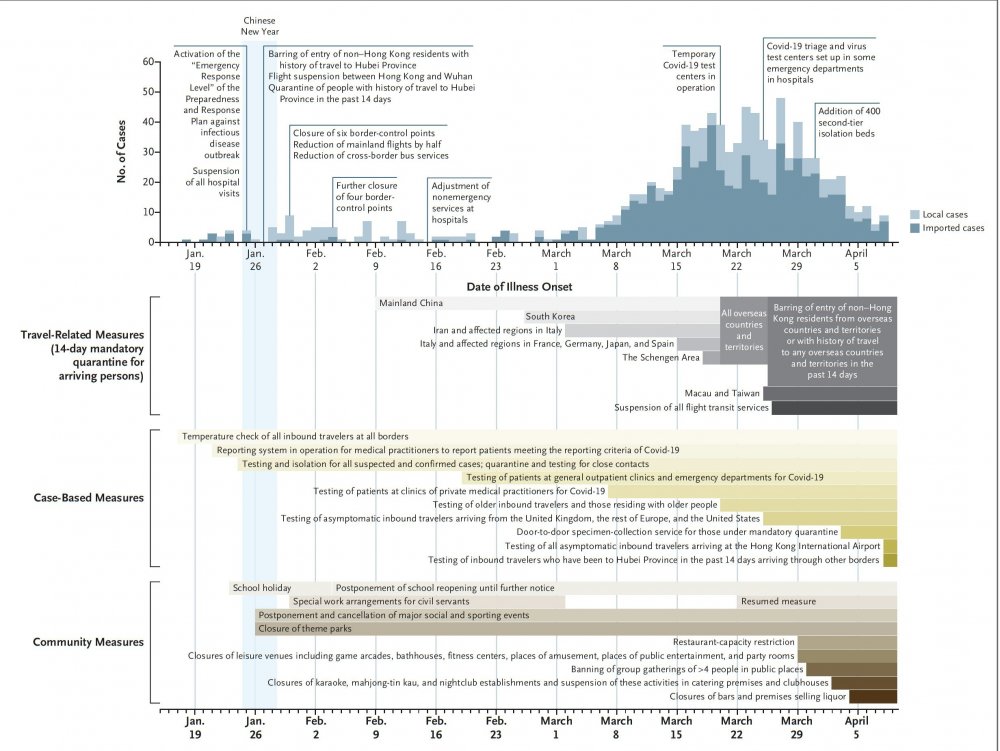
She emphasizes that: the figure with the seating plan is really impressive, so I’ll post it large
Figure 2. Floor plan of the 11th floor of building X, site of a coronavirus disease outbreak, Seoul, South Korea, 2020. Blue coloring indicates the seating places of persons with confirmed cases.